Bimonthly assessment for the month of Feb
Questions:Q.1) Please go through the patient data in the links below and answer the following questions:50 year man, he presented with the complaints ofFrequently walking into objects along with frequent falls since 1.5 years....Drooping of eyelids since 1.5 years...Involuntary movements of hands since 1.5 years ....Talking to self since 1.5 yearsMore here: https://archanareddy07.blogspot.com/2021/02/50m-with-parkinsonism.html?m=1Case presentation links:https://youtu.be/kMrD662wRIQa). What is the problem representation of this patient and what is the anatomical localization for his current problem based on the clinical finding.
Localisation of lesion:Drooping of eyelid is called as ptosis and our patient has Bilateral ptosis, which is because of weakness in levator palpebrae superioris or Muller muscle➡ muscle involvement➡Nucleus -centre caudal nucleus of occulomotor complex ...➡Nerve involvement( 3rd CN)https://www.sciencedirect.com/topics/medicine-and-dentistry/levator-palpebrae-superioris-muscle.self talk -frontal lobe of brain ....For involuntary movement : Basal ganglia ...https://stanfordmedicine25.stanford.edu/the25/im.html.b) What is the etiology of the current problem and how would you as a member of the treating team arrive at a diagnosis? Please chart out the sequence of events timeline between the manifestations of each of his problems and current outcomes.etiologyb/l ptosis-https://www.medicaleducationleeds.com/paces/ptosis/#:~:text=Differential%20Diagnosis%20of%20ptosis%3A,Horner's%20syndromeClassification Of ptosis✡➡NMJ : Myasthenia gravis⚛➡Neuropathic : 3 rd CN palsy , horner's syndrome⚛➡Mechanical lid tumors⚛➡myogenic : myotonic dystrophyThe size of pupils on examination is normal:therefore rules out horner's syndrome or 3rd CN palsy(as a single nucleus supllies both levator palpebral superioris ,its lesion causing b/l ptosis.)Mysathenia gravis -no history of fatigueable ptosis.Self talk - lesion at frontal lobe of brainSequence of events:Seizures 10 years back
--)Type 2DM 2 years back
--)Sudden blurring of vision while riding bike met with RTA -- fracture in left leg ,operated 2 years back
Frequently walking into objects along with frequent falls, drooping of eyelids, Involuntary movements of hands, Talking to self since 1.5 years.⬇⬇Non healing ulcer at surgical site 7 months back (post implant failure)⬇⬇Diagnosed as PSP & discharged with SYNDOPA 110mg & QUETIAPINE in kamineni, narketpally1 month back⬇⬇5 days later, patient presented to casualty in a state of unresponsiveness with GCS: 3/15 with H/o 2-3 episodes GTCS seizures.Another 2 episodes of generalized tonic seizures in casualty - treated with levipilSuddenly his saturations & heart rate dropped with no peripheral pulsations and patient was intubated - CPR done and was resuscitated.
Patient was put on mechanical ventilator - CPAP mode.
Later, weaning was done, GCS improved to 8/15.
Patient is still in ICU, and his vitals are monitored hourly.c)What is the efficacy of each of the drugs listed in his current treatment plan?No medication currently is known to be effective in PSP patient...Efficacy of Syndopa in the following link 👇https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2699657
Efficacy of Quetiapine in the following link 👇
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2699657/2 Q....Patient was apparently asymptomatic 2 years back then he developed weakness in the right upper and lower limb, loss of speech.Case presentation links:a) What is the problem representation of this patient and what is the anatomical localization for his current problem based on the clinical findings?
Problem representation:
A 60 year old man with a history of CVA 6 months back presented with
• Weakness in right upper and lower limb with loss of speech 2 years back.
•Shortness of breath since 2 months (grade 2 progressed to grade 4 ( on rest) with orthopnea and paroxysmal nocturnal dyspnea. )
•Bilateral pedal edema since 2 months
•Reduced urine output since 2 months
•Generalised weakness since 2 months
Anatomical localization :
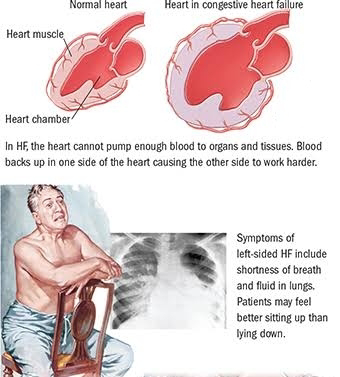
History suggests SOB grade 2 to 4 (even on rest), orthopnea and paroxysmal nocturnal dyspnea.Classical symptoms of left heart failure.Examination findings -•📍📍Pedal edema upto knee -- GRADE 2 (features of RIGHT HEART FAILURE too, due to back pressure)
📍📍His examination findings were Visible apical impulse, Pericardial bulge, visible pulsations, dilated veinsshift of apex beat to 6th ICS ..⚛Chest Xray PA shows Cardiomegaly
⚛His 2Echo is suggestive of Heart failure DCMP with Hypokinesia at RCA, LCX.
His Ecg shows poor R wave progressionAnatomical diagnosis:
The location to his problems is at the Heart, secondary to atherosclerosis of vessels.
b) What is the etiology of the current problem and how would you as a member of the treating team arrive at a diagnosis? Please chart out the sequence of events timeline between the manifestations of each of his problems and current outcomes.Etiology:CAD leading to DCMPECG showing :1)normal axis2)poor R wave progressionsuggest a CAD probably involving LAD and LCX.Etiopathogenesis :Alcohol overintake⬇⬇⬇Deranged lipid profile⬇⬇⬇Atherosclerosis of vessels⬇⬇⬇Affecting coronary vessels⬇⬇⬇Myocardial infarctionSequence of events:CVA ,2 years backandSOB, pedal edema, decreased urine output & generalized weakness since 2monthsandTreated with diuretics(aldosterone antagonist) and beta blockers ,ARBWith salt and Fluid restriction.c) What is the efficacy of each of the drugs listed in his current treatment planSalt and fluid restriction :Individualized salt and fluid restriction ( improve signs and symptoms of CHF ➡ in patients with moderate to severe CHF and previous signs of fluid retention.)https://www.sciencedirect.com/science/article/pii/S2213177915006551Benfomet as thiamine replacement in alcoholic patients. : helps in recovery frm longterm alcohol dependance..TELMISARTAN AND METOPROLOL:3Q. 52 year old male , shopkeeper by profession complains of SOB, cough ,decrease sleep and appetite since 10 days and developed severe hyponatremia soon after admission.Case presentation video:a) What is the problem representation of this patient and what is the anatomical localization for his current problem based on the clinical findings?
Problem representation:
A 52 year old man, who is a known to be a Diabetic and hypertensive presented with:
• Dyspnea since 10 days
• Productive cough since 2 days
• Disturbed sleep since 10 days
Anatomical localization:
The anatomical location of the problem is in the lungs (since grade 2/3 SOB without palpitations/chest pain/PND/orthopnoea can be attributed to lung problem)
Lower respiratory tract infection.
b) What is the etiology of the current problem and how would you as a member of the treating team arrive at a diagnosis? Please chart out the sequence of events timeline between the manifestations of each of his problems and current outcomes.
No respiratory examination has been mentioned in the elog.
However his problems list are:
Through RFT report and GRBS charting, we came to know abt patients respectively
- Hyponatremia
-Uncontrolled blood sugars
Through brief history :
-Dimorphic Anemia
-Lower respiratory tract infection
O/E - on examination of lower palpbreal conjuctiva -pallor+
Peripheral smear - microcyte/ + macrocytes, hypersegmented neutrophils are present )
Sequence of events52 year old with DM Type 2 and HTN⚡Developed symptoms of sob, cough, decrease in sleep and appetite, generalized weakness⚡Patient developed anemia (most common cause of anemia is NUTRITIONAL ANEMIA) with uncontrolled blood sugars.⬇⚡incidental findingHyponatremia (blood sodium levels = 121 mEq/L) is noticed.First -restricting fluids with minimal intake of hypertonic saline 3%🚩Calculation of the sodium deficit:0.6 x weight(kg) x (desired Na+ - Actual Na+). Use 0.5 for females. Desired Na+= 120-125 meq/l.Example: 70kg male. Na+= 110 meq/l Desired target= 125 meq/l.[0.6 x 70kg x (125-110)= 630 meq of Na+ needed].Amount needed to increase serum sodium level by 1 meq/l/hr= 0.6 x 70kg x 1.0= 42 meq/hr (safe rate for this patient).3%--hypertonic saline contains 513 meq/liter.Therefore: [desired rate per hr] / 513 x 1000 = infusion rate (ml/hr).And the total infusion time= [total meq needed] / [meq/hr]Desired rate= 42/513 meq x 1000= 82 ml/hrInfusion time= [630 meq] / [42 meq/hr] = 15 hrs.Therefore: Infuse 3% saline at 82 ml/hr for 15 hours.Source- https://globalrph.com/dilution/sodium-chloride/•Maximum correction for Na which can corrected in a day is 8-10 meq•First 4 hrs -4meq has to be corrected•Next 20 hrs -remaining calcuated Na should be given•we have to control sugars since for every 100mg increase in sugars, 1.6 Na will decrease (remembered as sweet 16)However in a type 2 diabetic we consider 124 too as normal Na range ..2) proper control of sugars with insulin and metformin.C) What is the efficacy of each of the drugs listed in his current treatment plan especially for his hyponatremia? What is the efficacy of Vaptans over placebo? Can one give both 3% sodium as well as vaptan to the same patient?1) Efficacy of vaptans over placebo :https://acsjournals.onlinelibrary.wiley.com/doi/full/10.1002/cncr.284682) Can one give both 3% sodium as well as vaptan to the same patient?No,We shouldn't give both at a time.Since there is a risk of over correction leading to hypernatremia.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5752787/4) Please mention your individual learning experiences from this month.I’ve seen many cases with :• Heart failure• COPD patients .. (Barrel shaped chest)• Alcohol dependance syndrome with tremors, alcoholic liver disease. Bells palsy• hemiparesis casesI’ve seen cases that are very rare, like:1. Progressive Supranuclear Palsy1. A 50 year man with Progressive supranuclear palsy.As an icu intern, patient GCS WAS 3/15 at arrival to hospital, being icu intern I checked his GCS score and monitored his vitals..2) 33 year old man with HFrEFPatient was admitted in icu fr one week, and on my duty day, I found TROUSSEAU's Sign positive... Aditya sir PGY3 appreciated my work..📍📍salt and fluid restriction in a maintainence hemodialysis patient and outcomes in the long run📍📍45 Y/F with severe anaemia...📍📍assisted in performing an pleural tap.📍📍I’ve done diagnostic ascitic tap for a nephrotic syndrome patient with ascitis.I’ve taken videos of case presentation and case discussion in 2-4 pm session, and uploaded them on YouTube .It was a heavily rewarding experience and i consider it my privilege to work with such experienced and enthusiastic doctors. I found it highly motivating and i have learnt so much.